Archives
All posts for the month January, 2014
January 26, 2014 | By Susan D. Hall
Article link: http://www.fiercehealthit.com/story/digital-divide-persists-health-it-adoption/2014-01-26?utm_medium=nl&utm_source=internal
Adoption of electronic medical records by primary care physicians has grown substantially, but the “digital divide” between large and small physician practices persists, according to a new study from the Commonwealth Fund.
Between 2009 and 2012, adoption grew from 46 percent to 69 percent. A majority of physicians use core health IT functions such as e-prescribing, electronic ordering of lab tests and certain types of clinical decision support.
Practice size, however, is the major factor affecting adoption. Ninety percent in practices of 20 or more physicians use EMRs, compared to just half of those in solo practices.
In 2012, 33 percent of primary care physicians could exchange clinical summaries with other doctors, and 35 percent could share lab or diagnostic tests with doctors outside their practice. Roughly one-third offered electronic access to patients.
Physicians who are part of an integrated delivery system, such as Kaiser Permanente or the Veterans Administration, practices that share resources or those eligible for financial incentives have higher rates of health IT adoption.
The report’s authors suggest that technical assistance programs and financial incentives can help close this “digital divide.” In addition, they say, physician practices remain behind schedule in their preparation for ICD-10.
In a recent survey of physician practices, 75 percent of respondents said they still haven’t started implementation of their ICD-10 transition plan, but still think they’ll be ready by the Oct. 1 deadline.
Meanwhile, new National Coordinator for Health IT Karen DeSalvo says the “next chapter” of the ONC’s work will focus on harnessing health IT for, among other things, population health: “[T]o see the promise of health information technology in the clinical interface for the health systems and the population and community at large to come to fruition,” she said at a recent Health IT Policy Committee meeting.
ONC and the U.S. Department of Health & Human Services Office for Civil Rights are developing a risk assessment tool due out later this year to help small providers navigate the privacy and security requirements suggested for Meaningful Use.
To learn more: – find the study
Related Articles: Health IT momentum must be maintained through ‘pivot,’ DeSalvo says Best practices for achieving HIMSS stage 7 Despite lagging on ICD-10 efforts, physician practices upbeat Hospital exec: Too many EMR features tied to billing ‘Next chapter’ of ONC’s work to focus on population health management, DeSalvo says
Read more: ‘Digital divide’ persists in health IT adoption – FierceHealthIT http://www.fiercehealthit.com/story/digital-divide-persists-health-it-adoption/2014-01-26#ixzz2rivPMKwm Subscribe at FierceHealthIT
NOVEMBER 18 2013
https://www.cerner.com/blog/whats_this_blue_button_thing/?langtype=1033
Blue Button: have you heard of it? If you keep an eye on health care or health IT social media, the term is almost impossible to miss. You may have heard other names such as ABBI, Blue Button+, Blue Button+ Direct, Blue Button+ REST, and Blue Button Connector.
So what is Blue Button? Since its inception in 2010, the term Blue Button has become overloaded and, to some extent, ambiguous. But no matter which definition you use, the underlying theme has always been the same: enabling consumers to have access to their personal health data. So follow me as I break Blue Button down into tangible and meaningful entities.
Blue Button: The Noun
The original Blue Button concept was born in the VA in 2010, and consisted of a simple text document containing personal health data that a consumer could download or view from the VA website. The definition of the term actually referred to the document itself and its contents and format. The format was a plain ASCII text file, but over the course of next two years, it evolved to support the more structured Consolidated CDA format with Meaningful Use Stage 2 specific fields.
If you think of this in terms of Farzad Mostashari’s now infamous noun vs. verb, Blue Button would have qualified as a noun. The ability to download the document was denoted with a blue button that was clicked to either download the document to persistent storage or to print it. Others soon followed suit and began to implement the document spec and offer the same ability download and print personal health data.
What does a consumer do with the data? That’s really beyond the scope of this post, but an important question nonetheless. Without use cases and workflow, the data is just data. If one were to just read the document content in raw format (let’s say over the phone to provide medical history to another provider), he or she may have trouble based on the limited formatting capability of a plain text document or understanding the sections of a C-CDA XML file.
In 2011, the VA held a Blue Button challenge to kick start innovation using the ASCII document format. In 2012 ONC issued the Blue Button Mash-Up challenge to build upon the initial challenge and champion a higher level of integration with other data and workflow. The winners of the latter challenge proved that data could be utilized in innovative and meaningful use cases, and was an important milestone for the growing patient engagement movement. In 2013, additional challenges were issued from various groups utilizing the latest Blue Button+ specifications pushing the envelope into the bleeding edge.
Blue Button+: The Verb
In the summer of 2012, a group gathered in Washington, D.C., to explore initiatives to accelerate patient engagement. The outcome was the creation of ABBI (Automate Blue Button Initiative), and their vision was to make it incredibly easy for a consumer to get access to their personal health data. This concept implied new use cases and workflows and quickly moved the context of Blue Button from a noun to a verb. Shortly after the project workgroups kicked off, the name was changed from ABBI to Blue Button+ indicating that the concept was a long-term initiative with goals expanding beyond automation. The workgroups focused on three main use case themes: download, push and pull.
The download and transmit use cases are modeled after the Meaningful Use Stage 2 VDT (view, download, and transmit) requirements. The download function is in line with the original Blue Button noun concept, with expanded data formats to match those of both Meaningful Use Stage 1 and 2. Data can be downloaded in one of the following formats:
- Consolidated CDA with MU2 fields and sections
- MU1 Continuity of Care Document/C32
- Human readable formats such as PDF, TXT, or a Microsoft Word DOC
The transmit functionality, now called called Blue Button+ Direct because of its use of the Direct Project as its transport specification, is aligned with the VDT transmit function. However, it’s a profiled approach to VDT, meaning it targets a very specific set of functional and technical requirements that are part of the VDT catalog plus a few additional requirements. Specific requirements include:
- The receiving Direct address of choice is a personal health system
- The message body specifies an optional text section indicating that the message was sent from a patient or on behalf of a patient’s request.
- Messages may be automatically sent based on systemic triggers, implementing the automate function of ABBI. Because the transmission of data to the patient can be triggered without the patient having to sign into a portal or request the information by other manual means, this can significantly simply the workflow from the patient’s perspective
- Blue Button-specific trust bundles are available for data holders and personal health systems. I described the importance of trust bundles in Direct exchange and patient engagement in my scalable trust story blog.
Through the remainder of 2012 and into early 2013, the workgroups formalized the Blue Button+ specification and published a detailedimplementation guide in February 2013. The good news is that if you were implementing EHR technology that included the MU2 VDT functions, you were already implementing a vast majority of Blue Button+.
It’s worth mentioning that the initial Blue Button+ Direct use cases only move data from the data holder to the consumer. Part of the reason was for simplicity and to accelerate adoption of the technology, but another is based on policy. The implementation guide contains privacy and security sections outlining the policy implications of the workflow, and the Blue Button+ trust bundle inclusion requirements were developed with these issues in mind. Currently, Blue Button+ Direct use case enhancements are being considering that include consumer-generated data being transmitted to data holders. The necessary security and privacy policies to support these use cases are also currently being investigated and developed.
As Blue Button+ Direct came to market, the Blue Button community sought other types of data and transport methods. Blue Button+ is now an umbrella for a growing portfolio of standards, which include not only the Blue Button+ Direct specifications, but also Blue Button+ REST and the Blue Button+ Payer workgroups.
The Blue Button+ REST specifications are built on contemporary technologies, some of which are still in IETF draft state or under IHE ballot consideration. They are based on the RESTful API paradigm and increase the number of data access methods and types of data that can be retrieved. The paradigm differs from Blue Button+ Direct in that the patient health system applications can programmatically access authorized patient data on demand instead of waiting for the data to be pushed from the data holder. To some extent, this puts the consumer in more control of when they access their data. The REST workgroup has completed their initial implementation guide, and is activity-seeking pilots from both data holders and personal health systems.
The Blue Button+ Payer workgroup recently kicked off as part of the Standards and Interoperability Framework. This effort will standardize financial data such as claims and evidence of benefits (EOB) for consumer purposes.
Blue Button Connector and The Movement
ONC is ramping up for a campaign that will kick off in January 2014 called the Blue Button Connector. It consists of a tool that helps consumers find providers and various entities that support Blue Button technologies. The connector will initially list providers that have successfully attested to meeting the MU2 VDT requirements and will list any provider, as well as data holders such as insurance companies, labs, and pharmacies. It will reveal what type of data patients can access, access options, support of automation triggers, and use of the Blue Button trust bundle. The connector will also enumerate personal health systems that can access and consume Blue Button data. ONC is also vigorously engaging data holders and other patient engagement activists to support the propagation of Blue Button, and holding a series of developer forums and competitions to encourage the development of personal health systems ready to receive Blue Button data.
From its inception, to now, and moving into the future, Blue Button is all about consumer access to person health data. It is constantly evolving to meet the challenges of today and tomorrow, both functionally and technically, with the vision of ubiquitous data liberation. Rather than aligning with a specific technology, the Blue Button term is moving towards a branding philosophy consisting of a portfolio of technologies and use cases. Consumers will simply associate the Blue Button brand with access to their personal health data.
Greg (@Greg_Meyer93) is a director and distinguished engineer at Cerner. He’s responsible for the HISP architecture of the Cerner Direct solution and remains actively engaged in development/coding and mentoring new software engineers and upcoming architects. Also responsible for the Direct Project Java reference implementation architecture and a primary source contributor, Greg serves as co-chair for the Direct reference implementation workgroup, is a contributing member of ONC’s Standards and Interoperability Framework initiative, and the Trust Bundle Operations workgroup lead with DirectTrust.org.
- Category: EHR, Technology, Direct Project, Interoperability
- Tags: Blue Button, Direct Project | Comments (0) | Rating: 5/5
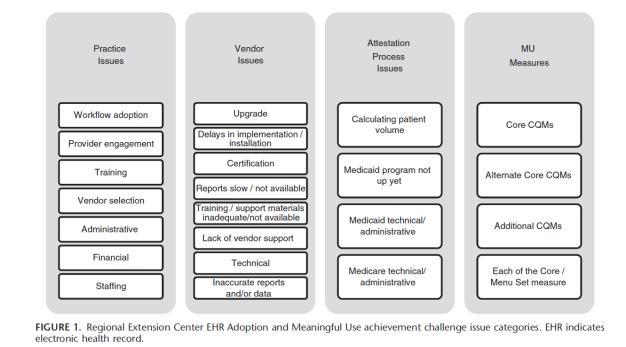
Background: Adoption and implementation of electronic health records (EHRs) has not been without challenges as it infuses technology into what has been a historically manual process of recording patient information. In an effort to identify these challenges, the Office of the National Coordinator for Health Information Technology leveraged the Regional Extension Center population of over 140,000 providers to develop a structured way to track challenges to EHR adoption and Meaningful Use (MU).
Objectives: This report summarizes challenges to EHR adoption and MU based on nationwide data supplied by 55 Regional Extension Centers reporting over 19,000 issues representing over 43,000 unique health care providers. Practices were grouped on the basis of their place in the lifecycle of EHR adoption and MU achievement.
Article link: http://www.healthcare-informatics.com/article/how-healthcare-organizations-can-turn-big-data-smart-data?page=2
It is important to remember that big data is more than just a sea of information; it is an opportunity to find insights in new and emerging types of data and content. So what are hospitals and healthcare organizations forgetting in their paths for eventual success with big data? According to Pilcher, the answer is “smart data.” In the below interview with HCI Assistant Editor Rajiv Leventhal, Pilcher talks about the difference between big data and smart data, strategies for collecting the right data, and advice for physicians in getting on board with the movement.
When you say “smart data,” what do you mean? How does smart data differ from big data?
The data that organizations are collecting today that they will be using for big data are going into this black hole (usually the data warehouse) somewhere. They are happy that they’re collecting it and preparing for when big data finally does come around to their organization, but if they aren’t careful and if they don’t monitor what they’re recording, the quality and quantity of the data when it’s to be used five years from now will not be sufficient enough. These organizations might think that they have five years of historical data to start their analytics, but in reality, the data is often not of the quality or quantity, or even the type, that is needed. That’s the smart data—that step that focuses on the type of data that they have, the volume of data, and also the validity of that data. You have to make sure that what you’re collecting is what you’re expecting.
Do healthcare organizations recognize this need?
Big data is a common theme with CIOs at healthcare organizations everywhere—they know it’s coming. However, there are CEOs at their hospitals who hear about “big data” at conferences and have no idea what it is, yet they will still come back and tell their CIOs that they “have to be doing big data.” And thus, it’s left in the lap of CIOs. But for the CIOs, they have Stage 2 of meaningful use and ICD-10 coming [for many providers, Stage 2 is here already], so they are not in the best place to be dealing with big data. So for the most part—except for about 5 percent of organizations out there, they tend to move it to sideline. It’s like looking at the side view mirror on your car and not seeing the message, “images are closer than they appear.” They see big data reflected, but it’s a lot closer than what they’re thinking. For the places that have limited resources and time, this is something that is being pushed to the side until they can get to it down the road.
How can organizations better ensure they are collecting the right quantity and quality of data?
First, you need to start developing your strategy now. Using the standard data models and approaches other industries are using doesn’t necessarily translate to healthcare IT. The amount of data, the data structure, and the data model is off the chart compared to even something as large as automotive manufacturing—the complexity isn’t even comparable. You have to develop as you go. The biggest thing I can suggest, as this industry is developing and our tools are growing, is to develop those peer networks with other healthcare leaders that are already further down the road than you. About 5 percent of healthcare organizations are right now in “stage two” of the data maturity model where they could start looking at predictive and prescriptive approaches to data. Those that are on the forefront of data analysis and intelligence are going to be critical to the rest of the industry following along. So learn from and use your peers.
And again, the quality of the data is critical. Organizations often think that they initiated the data collection, it’s implemented, and it’s working, so they turn to next project, thinking that when they’re ready, they will have it there in the warehouse. But then when it gets closer to the time to use the data, they don’t have the quantity that they thought they had. If you are collecting the wrong information or it’s incorrect, when you do your analysis, you will get wrong results and not even know it. Decisions could be devastating because your data was inaccurate leading to wrong analysis.
So you also need to assess the data on a regular basis constantly and ensure that what you think you’re collecting is actually what you’re getting. Then you can depend on the accuracy of that data when it’s time to start analyzing. Being able to analyze unstructured data for trends is very difficult, almost borderline impossible. Yet, about 80 percent of hospitals expect to use unstructured data in their data warehouse. Turning that data into structured data, or finding a tool that can do that for you with accuracy, becomes a huge push. If organizations are not prepared for that, they are racing against time at the last minute.
You need to trust the accuracy of your data. You know that your electronic health record (EHR) is collecting certain data and dumping into the data warehouse. But is anything happening with that transfer of data that is changing it in any way? Is it remaining accurate? Was it accurate to begin with? I wouldn’t say there is an issue of incorrect data in EHRs, but people can’t 100 percent say, “Yes, it’s ready to be analyzed.”
What are some other challenges organizations are facing with big data?
Time and money are the two big ones, of course. Everyone has a limited amount of time, with more projects and initiatives than time to do them in. And dollars are tight for healthcare organizations, so the things that tend to be more in the future get less priority when it comes to budgeting than things needed for today.
But staffing is also a problem—having trained staffs who know how to analyze and know how to approach intelligence processes can be challenging. A 2012 CHIME CIO survey, from last September, found that 67 percent of healthcare CIOs were reporting IT staff shortages. The issue is that organizations either didn’t have enough staffers, or didn’t have anyone internally with that skill set. At the end of the day, almost all organizations are having problems making up a BI department.
What is your advice to helping physicians get on board with big data?
This is definitely adding to the challenge for physicians. In many cases, a lot of them can view EHRs as taking up more of their time and causing more of a workload rather than being more efficient. Often, that is accurate. EHRs do not save you time, not at the beginning. And that’s why physicians tend to be resistant; they understand the need for meaningful use dollars, and that has pushed them in the direction, even though they have been reluctant to go there in the past.
But the day we can take that information and turn it into a tool for them to better take care of their patients, creating better outcomes at a lower cost, will be a benefit to all of the efforts and work they have been doing. That is why hospitals that have implemented BI initiatives; rather than just focus on the financial, they have to focus on the patient care strategies and initiatives. Because it’s not until then do doctors see a purpose for their extra work and start to get on board.
Article link: http://www.accountablecaremedia.com/wasden-we-have-created-an-ecosystem-of-useless-apps/
January 20, 2014 By Kristin Sims-Kastelein
NEW YORK—As an investor who has raised more than $50 million, Christopher Wasden managing director at PricewaterhouseCooper (PwC), has earned his controversial views on disrupting the current hospital and physician centric healthcare systems.
Christopher Wasden: Too often, we think that the doctor is the most important person in healthcare—the decision maker and the prescriber. In reality, the doctor is the last adopter. They are only going to adopt it once the consumer has shown them that it is valuable.
Some of these mHealth companies that initially tried to launch their service through doctors gave up and created a consumer version. It is actually easier to get consumer uptake than to get physician uptake.
Physicians see themselves as scientists. They need to have double-blinded, longitudinal studies. They are never going to use a device that isn’t paid for by an insurance company. There are huge barriers for doctors to drive this, whereas consumers don’t have to have clinical trials, and they don’t need insurance to pay for it. Once they have done it, then doctors will figure out a way to adopt it.
Increasingly, we have to ask ourselves how to create compelling consumer oriented value-propositions so we will hit a critical mass and so that doctors will now incorporate it as effective medicine.
ACO: There is a plethora of health and wellness apps in the marketplace. Where is mHealth in managing chronic conditions?
Wasden: It is not as if we are just starting to see disease-oriented apps. There are thousands of apps that claim to manage chronic conditions. There are more than 700 apps that say they control diabetes. Here is the issue: We have created an ecosystem of apps that are almost useless.
ACO: What can the mHealth market do to improve the quality of apps on the marketplace?
Wasden: There are six principles that drive the adoption of a successful mHealth app.
1. Integration: The app has to be integrated into the lifestyle of the patient and physicians have to integrate it into their workflow.
2. Interoperability: From a technological perspective, apps must share information and work across information technology systems.
3. Intelligence: It can’t just give you the data that you gave it. It needs to give you insights from the data that create changes in your behavior.
4. Social: You have to be able to share the information with a community that supports you in your behavior change.
5. Engaging: It has to be fun to use. You must want to use it and come back time and time again.
6. Outcomes: It has to collect information, show a change in behavior, and deliver better health outcomes.
If you look at the majority of apps out there, they don’t fulfill one of my six principles.
ACO: What is the reason that mHealth apps aren’t being built on these principles?
Wasden: Part of the reason is that the FDA is more likely to review your app before it gets issued to the public. I am not saying that this is right or wrong or good or bad, but a result of that is that a lot of companies say they would rather create a dumb app for a device so that it doesn’t have to get reviewed by the FDA and they won’t have to deal with regulatory issues.
ACO: What is your advice to mHealth developers?
Wasden: My advice is don’t be afraid of the regulatory approval process. Focus on the six principles that will create value in the health care ecosystem so that these apps become useful. At the end of the day, if we are not changing people’s behavior, we are wasting our time. Fifty percent of healthcare costs are associated with the wrong behavior. All of these technologies are all about changing the behaviors of consumers and clinicians.
ACO: Where do you see the market heading?
Wasden: The mHealth market has exploded, but it has exploded in volume not value. There are millions of dollars being made on apps. The vast majority is not bringing value.
We are moving from volume of apps to apps that are more valuable. As we do that, we will see consolidation, and effective apps will be integrated into other solutions.
Christopher Wasden is managing director of global healthcare innovation leader at PricewaterhouseCooper (PwC), where he advises clients on technology and business models that disrupt the current hospital and physician centric system and put consumers in charge of their healthcare experience. Prior to PwC, Wasden spent nearly a decade as a medical technology entrepreneur, raising $50 million in angel and venture capital; and several years working in public and private companies, leading their corporate finance.
Article link: http://www.forbes.com/sites/robertglatter/2014/01/19/us-gets-a-d-in-national-report-card-for-failure-to-support-emergency-patients/
The American College of Emergency Physicians (ACEP) released its Report Card last week measuring conditions and policies under which emergency care is delivered–unfortunately, the news is not so good. The nation earned a D+. In 2009, the last time ACEP’s report card was issued, America earned a C -. 
Dr. Alex Rosenau, President of ACEP, explained that the lower grade in 2014 reflects a misguided focus on cutting funding and resources for emergency departments because of the popular but erroneous view that emergency care is expensive–even though it represents less than 5 percent of overall US healthcare expenditures.
“Congress and President Obama must make it a priority to strengthen the emergency medical care system”, said Rosenau. “There were more than 130 million emergency visits in 2010, or 247 visits per minute”.
“People are in need, but conditions in our nation have deteriorated since the 2009 Report Card due to the lack of policymaker action at the state and national levels—the Report Card is a call to action”, added Rosenau.
As explained by Rosenau, the continued failure of state and national policies is jeopardizing patients treated in emergency departments. The Report Card also predicts increased utilization for emergency departments under the Affordable Care Act (ACA), while also describing the negative effects of shrinking resources and increased demand.
Dr. Jon Mark Hirshon, chair of the task force which drafted the Report Card, explains that the national grade for Access to Emergency Care has not shown improvement since 2009.
“America’s grade for Access to Emergency Care was a near-failing D- because of declines in nearly every measure”, said Dr. Hirshon. “It reflects that patients are not getting the necessary support in order to provide effective and efficient emergency care.”
“There were 19 more hospital closures in 2011, and psychiatric care beds have fallen significantly, despite increasing demand. People are increasingly reliant on emergency care, and primary physicians are advising their patients to go to the emergency department after hours to receive complex diagnostic work ups and to facilitate admissions for acutely ill patients”, Hirshon added.
It is important to emphasize that the Report Card measures the conditions and policies under which emergency care is delivered—not the quality of care provided by hospitals and emergency providers.
ACEP’s Report Card has 136 measures in five categories: Access to Emergency Care, Quality and Patient Safety, Medical Liability Environment, Public Health and Injury Prevention, and Disaster Preparedness.
The District of Columbia ranked first this year with a B-, pulling ahead of Massachusetts which held the top spot in the 2009 Report Card. Wyoming ranked dead last receiving an F.
The bottom line, according to Dr. Hirshon, is that the Report Card reflects the fact that hospitals are not receiving enough support to deliver efficient as well as effective care. Despite increased demand, there were 19 additional hospital closures in 2011. And with psychiatric and hospital inpatient beds declining as well, the system is compromising the care and safety of patients in the emergency department.
Based on findings of the Report Card, states continue to face many key issues such as workforce shortages, limited hospital capacity to meet the needs of patients, prolonged boarding periods for admitted patients (potentially compromising ongoing care), lengthy door to provider times, as well as prolonged emergency department wait times, not to mention increasing financial barriers to accessing care.
Twenty-one states received F’s in the category of Access to Emergency Care. In the Quality and Patient Safety Category, ten states received F’s, while in the Medical Liability category, ten states received F’s. In addition, ten states also received an F in the category of Public Health and Injury Prevention.
Even more concerning is that 13 states received F’s in the category of Disaster Preparedness: Delaware, Hawaii, Idaho, Illinois, Indiana, Montana, Maine, Utah, South Carolina, Vermont, Washington state, Wyoming as well as Wisconsin.
“Everyone hopes that their communities would preform as well as Boston did after the Marathon bombing, yet nearly half the states received either D’s or F’s for Disaster Preparedness, which is alarming” said Rosenau. “While there has been increased state and federal focus on disaster preparedness, there is great variability among states in terms of planning and response capacity”.
Key Recommendations of the 2014 Report Card:
- Fund the Workforce Commission, as called for by the ACA to evaluate shortages of physicians, nurses as well as other healthcare providers.
- Pass the “Healthcare Safety Net Enhancement Act of 2013”, providing limited liability protections to emergency and on-call physicians who perform services mandated by EMTALA, which requires emergency patients to be screened and treated, regardless of their ability to pay/insurance status.
- Withhold federal funds to states that do not support key safety legislation, such as .08 blood alcohol laws, and mandatory motorcycle helmet laws.